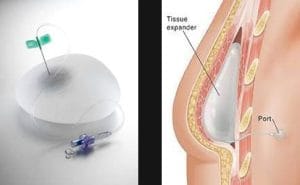
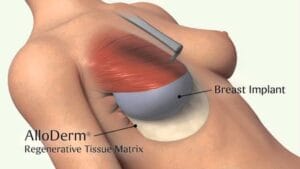
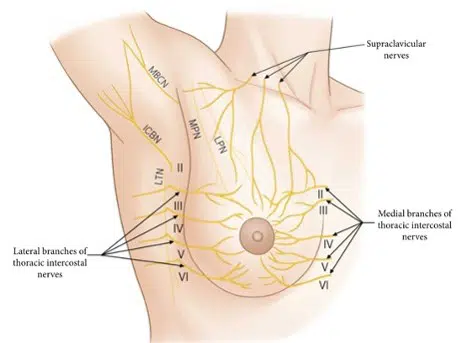
Breast reconstruction surgery is a surgical procedure to recreate the breasts after a mastectomy procedure has removed one or both of them.
Our Approach
We focus on the individual and utilize our knowledge and experience with all available reconstructive procedures to customize our treatment plan for each patient. We are not only experienced with performing the most complex breast reconstruction procedures, but we have also published numerous peer-reviewed journal articles to better understand and advance breast reconstruction. Our published peer-reviewed articles have covered multiple aspects of breast surgery, including:
- The most modern options for breast reconstruction
- Improving recovery following mastectomy
- Describing narcotic medication prescription patterns
- Assessing the risk for complications following breast reconstruction
We also believe that the most informed patients are the most satisfied with their reconstructive results. This is due to the shared decision-making between patients and physicians, which allows for the most ideal outcomes.